“Mitochondrial reverse electron transport in myeloid cells perpetuates neuroinflammation.”
Luca Peruzzotti-Jametti, et al. – University of Cambridge.
Background: Under inflammatory conditions, myeloid cells use reverse electron transport (RET) in mitochondria to promote generation of reactive oxygen species (ROS). While inhibition of RET provides in vitro anti-inflammatory benefits, it is unclear whether it could be therapeutic for inflammatory neurodegenerative diseases such as MS.
This Study:
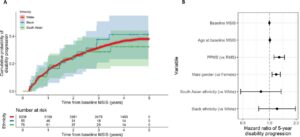
- Peruzotti-Jametti and colleagues found that expression of RET-related genes is increased during acute and chronic EAE.
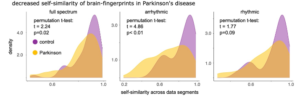
- Metabolic profiling found stark differences in microglia during acute and chronic phases. Acute-phase microglia showed higher levels of anti-inflammatory metabolites such as itaconate and GSSG, a byproduct of antioxidant reactions involving glutathione. Chronic-phase microglia showed both reductions in these metabolites and increases in indicators of oxidative stress such as creatine and citrulline.
- Microglia with induced RET generated greater levels of ROS and caused greater degeneration of neuron-like SH-SY5Y cells. The effects of RET induction were blocked by rotenone, an inhibitor of RET.
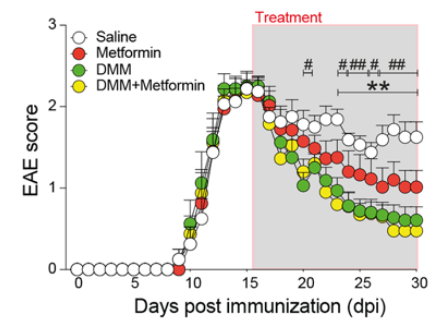
- Blocking RET in vivo by knocking out genes associated with generation of ROS led to significantly improved outcomes in an EAE model. Therapeutic benefits were also observed with administration of metformin or dimethyl malonate, which inhibit ROS production.
Bottom Line: Blocking RET-mediated ROS production may be a therapeutic target for treating MS, which might even be accomplished by repurposing the approved drug metformin.
Open Question: What is the broader impact of metformin having a therapeutic role by curbing ROS production? Could this help explain the observed link between metformin and reduced risk of AD?