Benedict Michael, et al. – University of Liverpool.
Background: While COVID infection has been associated with developing new neurological or psychiatric issues (NeuroCOVID), the long-term cognitive recovery trajectory for these and all other COVID patients remain underexplored.
This Study: Michael and colleagues compared 190 COVID patients with new onset neurological symptoms and 161 COVID patients without neurological symptoms, with normative data from 2,927 subjects, which was generated by drawing at least 8 subjects from a normative dataset matched for age, sex, first language, and educational attainment for each patient. The COVID patients were evaluated at entry into the study and 3-6 months after diagnosis.
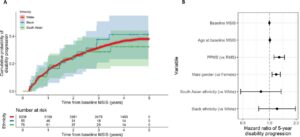
- Subjects with COVID infection history performed worse on cognitive assessments regardless of whether they had developed post-COVID neurological or psychiatric symptoms. These deficits were present in nearly all cognitive domains tested, the sole exception being that the non-NeuroCOVID (NN-COVID) patients lacked deficits in recognition memory.
- Both COVID groups (Neuro and NN) showed recovery between the initial post-acute assessment and their first follow-up appointment (median time interval = 111 days), but not between their first and second follow-up.
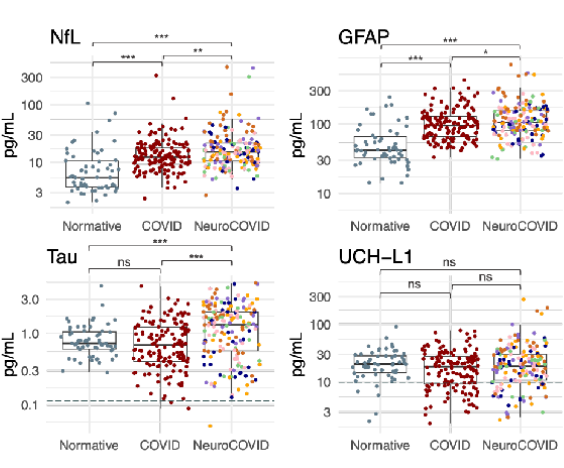
- Neurofilament light (NfL) and glial fibrillary acidic protein (GFAP) levels, two biomarkers for neural injury, were elevated in both COVID groups, with a further elevation in the Neuro-COVID group. The Neuro-COVID group also showed increased levels of total Tau.
- Bilateral anterior cingulate cortex volume negatively correlated with cognitive performance, suggesting changes to this region mediate cognitive deficits following COVID infection.
Open Questions: To what extent is this neurologic injury reversible? What are its long-term effects?
Bottom Line: Cognitive deficits appear to be a widespread phenomenon post-COVID, not restricted to those who developed severe neuropsychiatric symptoms.