Keita Hiraga, et al. – Nagoya University Graduate School of Medicine.
Background: While Alzheimer’s disease (AD) pathology is common in patients with Lewy body disease (LBD), it is unclear whether AD pathology begins to develop during the prodromal or symptomatic phase of LBD.
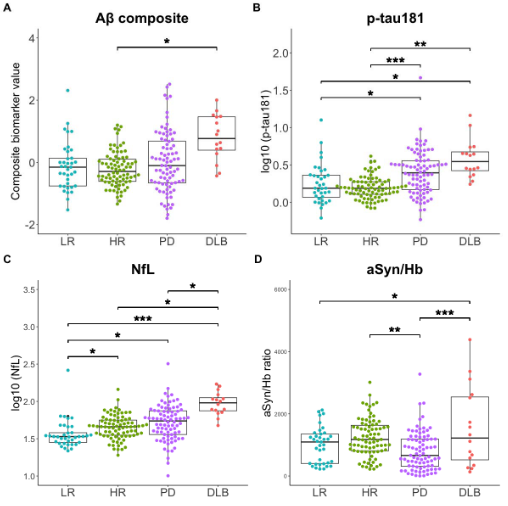
This Study: Hiraga and colleagues examined plasma levels of AD, PD, and neurodegeneration biomarkers in patients with PD, dementia with Lewy bodies (DLB), and healthy patients with (high-risk) or without (low-risk) 2 or more symptoms of prodromal LBD.
- Subjects were tested for levels of tau phosphorylated at residue 181 (p-Tau181), amyloid-beta composite (Aβ), neurofilament light (NfL), and alpha-synuclein (aSyn).
- p-Tau181 levels were elevated in both the PD and DLB groups, while Aβ levels were only elevated in the DLB group.
- High-risk subjects, as well as those in the PD and DLB groups, had higher levels of NfL than low-risk subjects, suggesting the onset of neurodegeneration during the prodromal phase.
- aSyn levels were reduced in the PD group compared to all others.
- In the PD group, Aβ and p-Tau181 levels were increased in patients with cognitive impairments compared to those without these impairments, suggesting a role for AD pathology in the cognitive effects of PD.
Bottom Line: AD pathology appears to play a key role in dementia associated with PD, beginning only during the symptomatic phase of LBD.
Open Question: Could intervening with anti-amyloid treatments during the prodromal phase of LBD reduce future cognitive symptoms?