“Translocation of gut commensal bacteria to the brain.”
Manoj Thapa, et al. – Emory University.
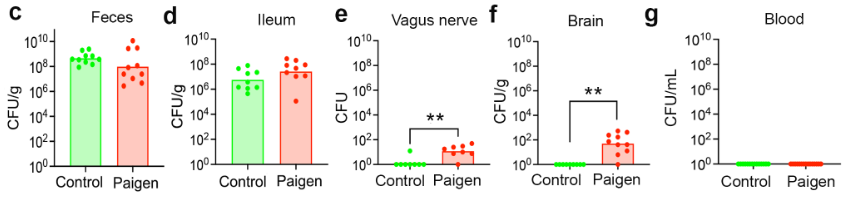
In this study, induction of gut permeability in mice led to the presence of commensal gut bacteria in the brain. This effect was observed when the gut was permeable due to diet as well as in mouse models of Alzheimer’s disease, Parkinson’s disease, and autism spectrum disorder, all of which have been reported to increase gut permeability. In multidrug resistance gene 2 (Mdr2) KO mice, commensal bacteria were also detected in the vagus nerve, with unilateral severing of the vague nerve sharply decreasing levels of these bacteria in the brain. Though absolute counts of bacteria in the brain were fairly low, they were sufficient to promote activation of microglia, potentially linking gut dysbiosis and permeability to neuroinflammation in the disease models tested.
While the data demonstrate the presence of bacteria in the brain and effects on resident microglia, they do not consistently support the model of transport via the vagus nerve. Out of 5 mouse lines tested and showing evidence of transmission, only two (Mdr2-KO and the autism spectrum disorder mouse model) showed significantly increased bacteria levels in the vagus nerve, with WT and Alzheimer’s model mice showing little to no vagus nerve bacteria. The authors do not address this issue, raising questions about how the gut bacteria are reaching the brain in these contexts when these bacteria cannot be detected in blood samples from these mice.