Overview
Donanemab
- Slows cognitive decline in Phase 3 trial, replicating Phase 2 results – John Sims
- Clears amyloid plaques, though effects on tau aggregates were not seen in primary analyses- Oskar Hansson
- Can cause serious side effects, like lecanemab, most notably ARIA- Stephen Salloway
- Reduces symptom severity – Liana Apostolova
- Is more effective than aducanumab- Andrew Pain
Other
- Eisai is working to deliver lecanemab SC, opening the door for patients to receive it at home via autoinjector- Brian Willis
- Future trials will test new anti-amyloids and new delivery methods – Paul Aisen
Presentation Summaries
As the first true disease-modifying therapy (DMT), lecanamab has the potential to revolutionize AD treatment, but the hunt is already on for the next DMT. Most prominent among these is donanemab from Eli Lilly, which revealed its Phase 3 trial results at the conference.
Donanemab slows cognitive decline, clears plaques
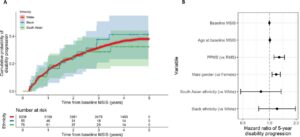
John Sims (Eli Lilly) shared what may have been the most anticipated data of the entire conference – a successful replication of the Phase 2 data revealing clinical benefits for donanemab. Among patients with low/medium tau, decline on the Integrated Alzheimer’s Disease Rating Scale (iADRS) slowed by 35% over 76 weeks, while decline on the Clinical Dementia Rating-Sum of Boxes (CDR-SB) slowed by 36%. The Phase 3 trial also included subjects with high levels of tau; when these subjects were included, the declines were slowed by 22% and 29%, respectively. This “weakened” slowing was mainly driven by the baseline decline being more rapid in high tau subjects, since the absolute differences between the treatment and control groups did not change. Once treatment group subjects cleared a sufficient amount of amyloid, active treatment was halted. On average, this occurred at week 47, with those discontinuing treatment still showing slower cognitive decline than subjects who never received donanemab.
Side Effects Similar to Lecanemab
Subjects given donanemab did experience significant side effects comparable to other anti-amyloid antibodies, as explained by Stephen Salloway (Brown University). When compared to placebo, the donanemab group had a higher rate of subjects discontinuing the study due to adverse events (13.1% versus 4.3%). Side effects included amyloid-related imaging anomalies (ARIA), with 24% experiencing ARIA-E (edema; 1.9% for placebo) and 19.7% experiencing ARIA-H (hematoma; 7.4% for placebo). Subjects homozygous for APOE4 had the highest rates of ARIA-E (40.6% versus 15.7% in non-carriers). Around 25% of ARIA-E cases were symptomatic, usually presenting as headache and/or confusion. Although 98% of ARIA-E events resolved, typically taking 10 weeks, 3 subjects in the donanemab group experienced severe ARIA and died, compared to 1 death in the placebo group considered related to treatment.
Clears Amyloid Plaques, but Questions Emerged Concerning Tau Aggregates
Oskar Hansson (Lund University) demonstrated that subjects receiving donanemab showed significant reductions in amyloid levels from the first measurement at 24 weeks based on imaging and fluid biomarkers. In the full cohort receiving donanemab, the percentage of subjects cleared of amyloid (<24.1 centiloids) at 24, 52, and 76 weeks were 29.7%, 66.1%, and 76.4%, respectively. Unlike in the Phase 2 trial, investigators found no difference in tau buildup within a portion of the frontal cortex; secondary analyses are currently underway to determine whether other brain regions showed reduced tau accumulation. In plasma, levels of tau phosphorylated at residue 217 (p-Tau217) were lowered by an average of 39.3%, with patients showing reduced p-Tau217 exhibiting greater cognitive treatment effects. In line with Phase 2 data, levels of glial fibrillary acidic protein (GFAP), a marker of reactive astrocytes, were also reduced. There was no clear pattern to changes in neurofilament light (NfL), a marker of neurodegeneration, with the donanemab group presenting higher NfL levels at 24 weeks, then going lower than placebo by a statistically insignificant amount. On the whole, these data affirm that donanemab is effective in curbing amyloidosis.
Slows Development of Dementia
What do these results mean for patients? Liana Apostolova (Indiana University School of Medicine) translated the data into clinical impact. On the iADRS, subjects receiving donanemab saved 4.4-7.5 months over an 18-month period, depending on which values are used. This means that the decline they experienced over 18 months was equal to the decline the placebo group experienced over 10.5-13.6 months. On the CDR-SB scale, the 0.67 point difference meant they generally experienced mild symptoms instead of moderate ones; for example, their memory impairments would be described as “consistent slight ‘benign’ forgetfulness” as opposed to “moderate memory loss that interferes with everyday activities.”
On the whole, donanemab appears to be another clinically effective tool for slowing the progression of Alzheimer’s. With Eli Lilly expecting to hear from the Food and Drug Administration by the end of the year, patients may soon have a new option for treatment.
Subcutaneous lecanemab could be much easier to deliver and reduce side effects
One of the chief limitations of lecanemab is the need for IV delivery, limiting the rapid, widespread deployment of anti-Alzheimer’s DMTs. To this end, Brian Willis presented data from Eisai’s efforts to deliver lecanemab subcutaneously (SC). A primary obstacle to this is that many SC vehicles require a fixed dose, whereas IV infusions have been dosed by patient weight. Fortunately, a fixed dose of 720 mg via vial & syringe achieved a pharmacokinetic profile similar to the standard 10 mg/kg dose via IV, with nearly identical effects on clearing amyloid and a comparable average steady-state concentration. Beyond SC being more convenient, it may prove less prone to causing ARIA-E by reducing the maximum steady-state concentration in the bloodstream.
What’s next?
The arrival of donanemab immediately raises the question of how it compares to lecanemab. Though head-to-head comparison trials have not yet been done, Andrew Pain (Eli Lilly) presented data from an ongoing clinical trial comparing donanemab to aducanumab, the first anti-amyloid antibody to receive accelerated approval from the FDA. This randomized, open-label trial, TRAILBLAZER-ALZ 4, has so far found donanemab to be the far more effective treatment, clearing amyloid faster and more effectively. Even after 12 months, the amount of amyloid cleared by aducanumab (56.1 centiloids) was less than the amount cleared by donanemab in just 6 months (64.0 centiloids), although this difference was not statistically significant (p=0.056).
Donanemab also had a more favorable safety profile, with fewer instances of amyloid-related imaging abnormalities-edema (ARIA-E). We will need direct comparisons with lecanemab to inform treatment decisions.
These comparisons involve providing anti-amyloid therapies during the early stages of cognitive decline. Given that amyloid buildup starts decades prior to symptoms, however, could treatment prior to symptom onset prevent them from occurring? Paul Aisen (USC) reported that Phase 3 trials to test this are underway for donanemab (TRAILBLAZER-3) and lecanemab (AHEAD). The amount of time needed to answer this question, however, means that primary data collection in these trials will not be completed until October 2027. Meanwhile, more DMTs are in the pipeline. Remternetug, Eil Lilly’s follow-up to donanemab, will complete preliminary data collection for Phase 3 trials in October 2025. The other antibody Aisen discussed, trontinemab, represents something of a second chance for gantenerumab, which failed its Phase 3 trial in 2022. Hoffmann-La Roche created trontinemab by fusing gantenerumab to an antibody fragment targeting the human transferrin receptor, in hopes that it will pass through the blood-brain barrier more effectively and clear more amyloid, as a similar fusion did in preclinical mouse models. Phase 1b/2a trials for trontinemab are currently underway.
Conclusion
The 20-year drought for new treatment options in AD has ended, moving beyond symptom management approaches to true DMTs.
For more on other DMTs under development, read our summary on novel therapeutics.