Editor’s note: many of the presentations on glia discussed connections with APOE. You can find coverage of those talks here.

Overview
Glia
- Risk factors for sporadic AD linked to how glia respond to amyloid plaques – Bart De Strooper
- Microglia and astrocyte activation peaks at start of MCI, microglia rebound in AD – Paul Edison
- Microglia, astrocyte activation, AD pathology linked early in disease progression – João Pedro Ferrari-Souza
- Glypican 4 required for astrocytes to take up tau and impair synapses – Claudio Grassi
Presentation Summaries
Neurons are often at the center of attention for Alzheimer’s; they are the cells that form amyloid plaques, develop tau tangles, and die off over the course of the disease. From the first observations by Alois Alzheimer, however, it has been clear that glia also undergo changes in AD. In this summary, we discuss presentations outlining these changes, including those adding to the growing body of evidence that glia play an active role in the disease.
“You get Alzheimer’s disease not because of the amyloid plaques, but because of the way your brain cells deal with them.”
This provocative assertion was how Bart De Strooper (VIB Center for Brain & Disease Research) concluded his presentation on human microglial responses to amyloid plaques. He began by pointing out that while the 4 “causal” genes for AD (APP, PSEN1, PSEN2, SORL1) are expressed in neurons, the majority of “risk” genes are expressed in non-neuronal cells. Microglia change their expression of these risk genes in mice with solely amyloid pathology, but not in those with solely tau pathology. Importantly, about 30% of AD risk genes lack an ortholog in mice. How can researchers study these human-specific mechanisms?
De Strooper addressed this challenge by developing MIGRATE, a protocol for xenografting into mice human microglia derived from embryonic stem cells (hESC). At the proteomic level, these transplanted microglia more closely resemble microglia collected directly from patients than those from mice or non-xenografted hESC microglia grown in vitro. RNA sequencing revealed that xenografted human microglia exhibit the wide range of expression profiles observed in mouse microglia, including cytokine-producing, antigen-presenting (HLA), and “disease-associated” (DAM). When transplanted into mice carrying the Swedish, Iberian, and Arctic mutations to amyloid precursor protein (APPN-L-GF) with amyloid pathology, more microglia entered these 3 states, at the expense of homeostatic microglia.
The next step is to compare human microglia from different genetic backgrounds following transplantation. Currently, De Strooper is studying 5 cell lines from subjects spanning the polygenic risk spectrum. While he stressed that the data were highly preliminary, there were clear differences in the proportions of microglia occupying each cell state, with the proportion of DAM microglia increasing with polygenic risk. If these results hold up, they support his assertion that individuals can remain healthy even when plaques are present if their microglial response does not induce pathology.
Trajectories of microglial activation and astrocyte reactivity
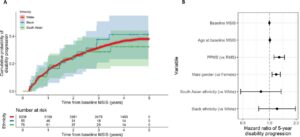
Paul Edison (Imperial College London) discussed how microglia and astrocytes change their (re)activation states along the AD progression timeline. Microglia become activated in early mild cognitive impairment (MCI), reduce their activation as MCI progresses, then consistently ramp up once patients reach the AD stage. At the first activation peak, higher levels of microglial activation correlate with greater grey matter volume, suggesting that this phase may represent a protective phenotype. (This is in line with Oleg Butovsky’s findings that microglial activation can be neuroprotective by promoting clearance of amyloid and apoptotic neurons; read more here.) Astrocyte reactivity, on the other hand, has a single peak centered around the beginning of MCI, with greater reactivity correlating with harmful phenotypes such as greater amyloid deposition, lowered glucose metabolism, and reduced grey matter volume.
Separating microglial activation and astrocyte reactivity into discrete events, according to João Pedro Ferrari-Souza (Universidade Federal do Rio Grande do Sul), ignores the extensive cross-talk between these two glial types. (For example, see Oleg Butovsky’s discussion of astrocytic control over microglial activation here.) To explore the association between the two, he examined data from subjects in the TRIAD cohort for levels of amyloid, tau, microglial activation, astrocyte reactivity, tau phosphorylated at residue 217 (p-Tau217), and cognitive assessments. Plasma p-Tau217 correlates with astrocyte reactivity, as measured by plasma glial fibrillary acidic protein (GFAP), only in subjects positive for activated microglia. No relationship was observed between tau aggregation, as measured by positron emission tomography (PET), and astrocyte reactivity, regardless of microglial status. However, tau aggregation did correlate with microglial activation in regions that accumulate tau late in AD progression (Braak III-IV and V-VI).
This suggests that microglia and astrocytes interact early in Alzheimer’s pathology, but not later. In light of Bart De Strooper’s findings, this could be explained as amyloid buildup only promoting astrocyte reactivity when activated microglia are exhibiting a harmful response to those plaques. In turn, the link between microglial activation and late, but not early, tau accumulation may relate to the second wave of microglial activation described by Edison that occurs once patients progress to AD.
Tau spread to astrocytes affects synapses
Models of tau pathology spreading across the brain often focus on neuron-to-neuron transmission. Claudio Grassi (Università Cattolica del Sacro Cuore) presented research on the impact of neuron-to-astrocyte transmission on synapses. Prior work from his group found that incubating astrocytes with oligomeric tau (oTau) for just 1 hour reduced their ability to open intracellular calcium (Ca2+) stores in response to ATP, take up glutamate, and release neuro/gliotransmitters, weakening the synaptic connections between co-cultured neurons. Knowing that heparan suflate proteoglycans (HSPGs) are often important for taking up proteopathic seeds, he explored the role for glypican 4 (GPC4), an HSPG expressed in astrocytes that is critical for excitatory synaptic function. Blocking GPC4 via an antibody reduced the ability of astrocytes to take up oTau, as well as the associated effects on intracellular Ca2+ and calcium-dependent ATP release. This blockade also prevented tau from reducing synaptic protein levels, impairing LTP induction, and weakening synaptic connections. Together, these results suggest that astrocytic uptake of oTau via GPC4 is a key factor for synapse loss in AD. Since tau pathology and synapse loss occur later in the AD time-course, astrocytes have an active role in late-stage pathology, even if they are not necessarily reactive.
Conclusion
These studies offer important insights into how glia factor into AD. Understanding how glia fit into Alzheimer’s is essential for developing effective treatments.